Many Synaptic clients integrate pelvic floor physiotherapy into their plans for recovery and into the quest to improve their quality of life. In this month’s blog we learn about how the bladder works. We talk about the types, causes, and treatments of Urinary Incontinence. Finally, we look at we can do to manage urinary incontinence with lifestyle advice to improve bladder control and pelvic floor physiotherapy exercises.
Urinary incontinence, or the involuntary leakage of urine, is a highly prevalent pelvic health concern both within Canada and globally. Research suggests that as many as 50% of women will experience urinary incontinence at some point in their lifetime. Pelvic floor dysfunction is not just a women’s health concern as 1 in 9 men in Canada will also have to cope with unwanted urine leakage. Although these symptoms are common, they are not normal! It is a common misconception to think that there is nothing that you can do about these symptoms, in particular after childbirth or with aging.

What is Urinary Incontinence?
Urinary incontinence, or the involuntary leakage of urine, is a highly prevalent pelvic health concern both within Canada and globally. Research suggests that as many as 50% of women will experience urinary incontinence at some point in their lifetime. Pelvic floor dysfunction is not just a women’s health concern as 1 in 9 men in Canada will also have to cope with unwanted urine leakage. Although these symptoms are common, they are not normal! It is a common misconception to think there is nothing you can do about these symptoms after childbirth or with aging, injury or disability.

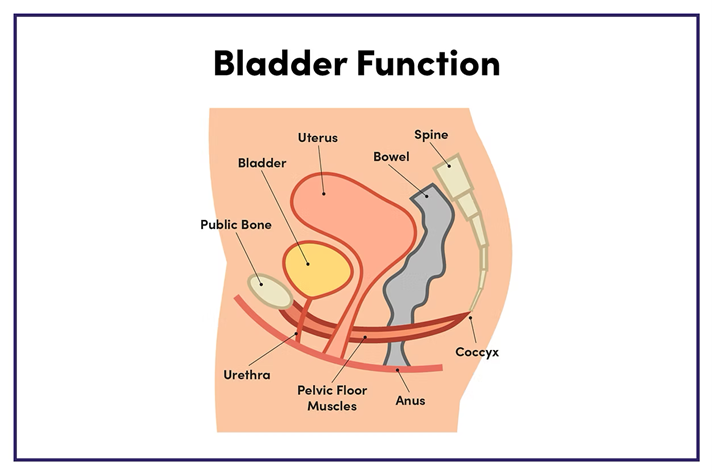
Bladder Function
To have full control of our bladder, two things are required: an intact central nervous system and properly functioning lower urinary tract and pelvic floor muscles. The pelvic floor muscles and the bladder muscle work together, but in opposite fashion. During the storage phase of urine production, the bladder muscle is relaxed while the pelvic floor muscles are contracted (to produce a closing pressure on the urethra). The opposite occurs when we want to eliminate - the bladder muscle contracts, while the pelvic floor muscles relax and lengthen to ensure opening of the lower urinary tract. Incontinence occurs when the muscles of the bladder and pelvic floor don’t function optimally, or if reflex control by the central nervous system is impaired.
Types of Urinary Incontinence
There are three common types of urinary incontinence:
- Stress Urinary Incontinence - Stress urinary incontinence is the most prevalent type and it is defined as the involuntary loss of urine secondary to an increase in abdominal pressure. This commonly includes sneezing, laughing, coughing, physical activity (lifting or jumping) and/or transitional movements.
- Urge Incontinence - Urge incontinence involves the sudden, urgent and sometimes unstoppable need to urinate.
- Mixed Incontinence - As the name suggests, mixed incontinence is the combination of symptoms of stress and urge incontinence.
Causes of Urinary Incontinence
Incontinence can occur for a variety of reasons. Urinary tract infections, vaginal infections or irritation, constipation or medication use can cause short term bladder control problems. When incontinence lasts longer, it could be the result of:
- Pregnancy and giving birth. Having had multiple children or obstetric trauma (use of forceps, suction or tearing) can increase the risk of incontinence. It is a common misconception that having a Caesarian section delivery protects the pelvic floor tissues from injury.
- Pelvic organ prolapse, which is the descent of internal organs (bladder, rectum or uterus) into the vaginal canal due to loss of strength and support from the pelvic floor tissues.
- Gynecological, abdominal, or urinary surgeries, including hysterectomies in women and prostatectomies in men.
- Chronic smoking or cough.
- Obesity.
- Heavy weightlifting or physically strenuous job.
- Aging. The prevalence of urinary incontinence increases with age in both men and women.
- Prostatitis, inflammation of the prostate gland, or Benign Prostate Hyperplasia (BPH), enlargement of the prostate gland, can cause incontinence in men.
- Chronic straining to eliminate, which creates excessive pressure downwards that can result in pelvic floor muscle injury.
- Neurogenic bladder, caused by damage to the nerves that control the bladder from injury or disease such as Multiple Sclerosis, Diabetes, Parkinson’s Disease or Spinal Cord Injury.
Treatment for Urinary Incontinence
Treatment for urinary incontinence depends on the type of bladder control problem, the severity of incontinence, and the best fit for your lifestyle. As a rule, conservative treatment options, including pelvic floor physiotherapy, should be first line treatment before surgery and other more invasive procedures are considered.
Lifestyle Advice to Improve Bladder Control
- Sip, don’t guzzle fluids!
- Limit drinking large quantities of fluids before to bedtime.
- Ensure adequate hydration - it is a misconception that drinking less water will improve bladder control! A decrease in liquid intake results in a decrease in the volume of urine; smaller urine volumes are more highly concentrated and irritating to bladder tissues. This may cause you to go to the washroom more frequently and encourages the growth of bacteria.
- Avoid/minimize bladder irritants like smoking, alcohol, caffeine, spicy foods, vinegar, artificial sweeteners, tomato-based products and food colourings.
- Choose water over other beverages.
- Prevent constipation, which acts as a blockage that could create pressure on the bladder, limiting its capacity to fill and causing irritation.
- Sit completely on the toilet to ensure that your pelvic floor muscles can relax and lengthen when urinating. This can be helpful for men to consider as well. Don’t rush and avoid “power peeing” by straining to urinate quickly.
- Walk, don’t run, to the washroom when you experience urgency. Stress is a contributing factor to urge incontinence, so trying to rush to the washroom quickly can make the sensation worse. Remain calm and perform deep breathing exercises while you make your way to the washroom to urinate.

Pelvic Floor Physiotherapy Exercises
Urinary incontinence may either be the result of pelvic floor muscles that are too weak or too tight.
If the pelvic floor muscles are too weak, it means that the tissues are not strong enough to provide support for our internal organs, including the bladder. The tissues cannot produce enough of a closing pressure around the urethra to provide adequate voluntary control of urination, resulting in leakage. Exercises to strengthen the pelvic floor muscles, including Kegels, bridges and bird dogs, can help to increase the bulk of core muscles to improve bladder control.
If the pelvic floor muscles are too tight, it means that the tissues have limited capacity to contract further when we experience increases in intraabdominal pressures, and/or the bladder has less capacity to fill. Exercises to lengthen the pelvic floor tissues, including cat/cow, child’s pose and happy baby, can be helpful to eliminate symptoms of urge incontinence.
In addition to bladder control training and lifestyle considerations, always speak to your physiotherapist and medical doctor about the most appropriate methods to improve your bladder control.
CONTRIBUTED BY:
Ellen Incognito - PT, MScPT, BScKin (Honours) Registered Physiotherapist


.png)

